Hermaphroditism and homosexuality in nineteenth-century America
[F]rom the anatomical point of view, the hermaphrodite is neither a monstrosity nor a freak of nature, but a creature devoid of ordinary development, that is, not developed sexually in conformity to its species. Physiologically, the hermaphrodite is a degenerate, impotent and sterile, imperfect in impulse and characteristic equilibrium, on account of unstable and perverted sex (1892).
So wrote an anonymous author in an 1892 medical journal. By the late nineteenth century, hermaphrodites (a historical term used to describe those born with discordance among the multiple components of sex anatomy: internal reproductive organs, external genitalia, and chromosomes) were no longer ostensibly considered “monstrous” or “freaks of nature,” though they continued to inspire a mixture of pity, disgust, and fascination, even among medical men, who we might have expected to be dispassionate about anomalous bodies. In colonial America, before surgery became an option to “fix” what was “wrong,” early interpreters saw unusual genitals as evidence of nature gone awry. Ministers and medical practitioners saw providence or the diabolical in “monstrous births.” And mothers were often blamed for their babies’ anatomies, for folk wisdom taught that maternal imagination could cause all kinds of birth anomalies. Medical men, and midwives as well, made pronouncements about gender that had extensive legal ramifications—whether to settle cases of bastardy or impotence, confirm or deny rape accusations, or substantiate divorce proceedings.
These early discussions of atypical genitalia tended to assume the immutability of sex. One was either male or female, and in cases where the physical appurtenances of sex suggested ambiguity, most commentators simply reverted to the language of deformity. Medical jurisprudence manuals and gynecological treatises of the eighteenth century generally doubted the existence of hermaphrodites as they were then defined: having a complete and perfect set of male and female sexual organs. Medical men instead insisted that many so labeled were simply women with enlarged clitorises. The mistaken belief in hermaphrodites, some medical authorities suggested, was due to ignorance of human anatomy, particularly that of the female. If hermaphrodites were really women with large clitorises, then their condition could lead to two evils: it could hinder coitus and promote sexual relations between women.
By the early nineteenth century, newly authoritative and professionalized physicians took the liberty of assigning a gender to people (not just infants) with uncertain genitals, even if that assignment opposed the patient’s preference and contradicted that individual’s previous gender performance. Like the rest of nineteenth-century society, doctors held the institution of marriage in high esteem and attempted to create genital organs that might accommodate normative marital relations. There were also legal reasons for “proving” that patients were either male or female, whether the question was one of enfranchisement, inheritance, or divorce. The existence of chromosomes or hormones was not yet known, nor was inspection of internal gonads then possible. Confounded physicians could but observe the often contradictory genitalia, and consequently their pronouncements depended as much on traditional stereotypical social indicators as on biological markers when they decreed a physically anomalous individual male or female. Nevertheless, decree they did, for convention required that a person be clearly male or female.
In the last decades of the nineteenth century the controversy over the definition of hermaphroditism intensified. The nineteenth-century medical journal articles can be interpreted as conversations amongst doctors, as they read and rebutted each other’s work. Often physicians referenced previously published cases in order to buttress their own opinions. The cases concerning hermaphroditism were no exception. Doctors cited sixteenth-century precedents, for example, in order to prove to their colleagues that hermaphrodites did not exist, despite the cases of ambiguous sex that they continued to see. The patients they evaluated, then, were “really” men or women, and doctors published their unusual cases to prove their points and validate their medical authority. Despite their fundamental disagreement over whether or not there was such a thing as a true hermaphrodite, these doctors had much in common. Most of them asserted their own importance in making decisions regarding their patients’ genders. Most of them wanted to see their patients involved in heterosexual relationships, especially marriage. And, much like the above anonymous medical manual contributor, most of them associated hermaphroditism (to the extent that they admitted its existence) with sexual perversion.
The (Im)possibility of Perfect Hermaphrodites
Although medical men wanted to ensure the specificity and stability of each person’s sex, uncertainties regarding the criteria for femaleness or maleness abounded in the nineteenth century. Were there people for whom sex could not be firmly established?
In Samuel Farr’s 1787 medical jurisprudence textbook, published in America in 1819, “perfect” hermaphrodites were defined as those “partaking of the distinguishing marks of both sexes, with a power of enjoyment from each.” Whereas earlier writers had required a perfect complement of parts to qualify as a hermaphrodite, Farr pushed the definition a crucial step further by adding “a power of enjoyment.” Hermaphrodites had to have both sets of organs and had to be able to use either one for sexual satisfaction. Could a hermaphrodite derive sexual pleasure as both a female and a male? That seemed impossible to most writers, though they revisited the question repeatedly throughout the eighteenth and nineteenth centuries. More than one nineteenth-century commentator also wondered if hermaphrodites would be able to impregnate themselves. But medical men were sure the answer was no. No such instance had ever been found.
By the mid-nineteenth century, some American doctors had become familiar with the sorting and stabilizing efforts of Isidore Geoffroy Saint-Hilaire, author of Histoire des anomalies de l’organization, published in 1832-1836 and soon excerpted in English in Theodric Romeyn Beck’s prominent medical jurisprudence textbook of 1838. Geoffroy Saint-Hilaire argued that hermaphroditism, per se, did not exist; as Beck translated the passage: “the external organs (as a penis and clitoris) have never been found perfectly double.” Geoffroy Saint Hilaire believed that anatomists had resolved the debate about hermaphroditism once and for all; he concluded that “it is anatomically and physiologically impossible.” Echoing Geoffroy Saint-Hilaire, John North, author of a two-part article on hermaphroditism and other “monstrosities” published in America in 1840, also denied the existence of perfect hermaphrodites. “Although we see many instances of true hermaphroditism in the animal and vegetable kingdoms,” he remarked, “no such cases have ever existed in the human subject; no human hermaphrodite, in the proper sense of the term, has ever existed; not a single so-called hermaphrodite in man has even been capable of performing the sexual functions of both sexes.”
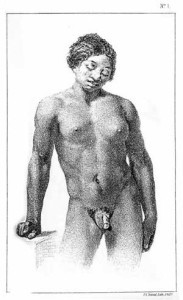
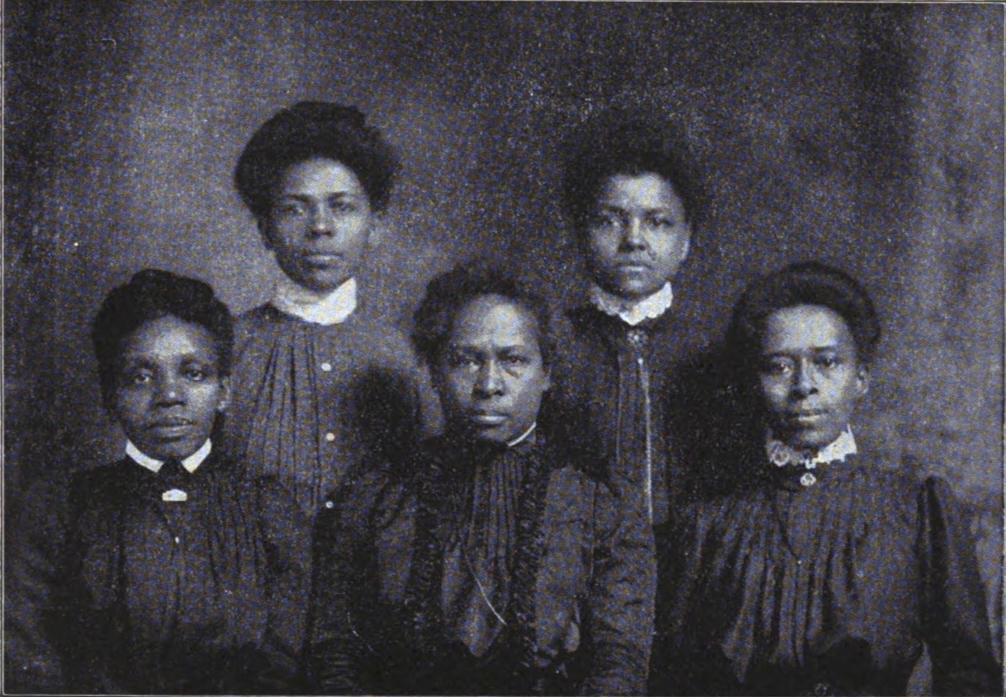
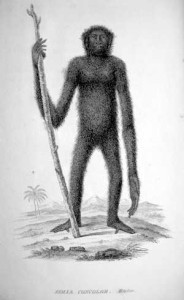
But despite assertions to the contrary, some physicians were convinced that the people they saw were indeed hermaphrodites, though they sometimes tempered their assertions by labeling a person a “spurious,” “false,” or “pseudohermaphrodite” if their external genitalia did not align with their internal anatomy. In 1850, Dr. Jonathan Neill, a professor of anatomy at the University of Pennsylvania, presented a subject who he believed was “certainly entitled to the term hermaphrodite.” The person, already deceased, arrived at the anatomical rooms of the university for an autopsy. Not much was known about the subject, other than that she “resided among the degraded blacks in the lower portion of the city,” according to the coroner’s jury, and that she died of “drunkenness and exposure.” The jury was able to surmise from her teeth and “general appearance” that she was between twenty-five and thirty years old when she died. Though the subject dressed in women’s clothes, Dr. Neill was not entirely persuaded that she was female. She had large breasts and no hair on her face, two markers that typically would indicate femaleness. But other secondary sex characteristics suggested maleness. Neill wrote that if one looked only at the ratio of the broad shoulders to the narrow hips and also at the shape of the limbs, it would “have indicated the male sex.”
What were the definitive markers of sex, then? Did large breasts and a smooth face trump narrow hips and broad shoulders? Upon inspection, the genitalia revealed a similar ambiguity. Dr. Neill said that from a “superficial view” of her genitals, “almost any one would have pronounced the subject to have been a hypospadic male.” (Hypospadias is a condition whereby the urethral opening is not at the tip of the penis, but underneath instead. In severe cases, the opening falls closer to the scrotum, which can resemble the labia majora.) Since this person was dead, Dr. Neill could go beyond the superficial and perform an autopsy to search for other clues. Inside the body, Neill discovered female reproductive organs: uterus, fallopian tubes, small ovaries, and a narrow vagina “of the proper length.” Now considered more female than male, Neill classified the subject’s condition as “spurious hermaphroditism in the female.”
Five years later, doctors France Wharton and Moreton Stillé mentioned the case in their textbook, A Treatise on Medical Jurisprudence. What Neill thought most would have seen as a hypospadic penis, Wharton and Stillé described as both a long clitoris and a penis. In an unusual display of uncertainty, the two described the subject as having a clitoris five inches long in one sentence and a penis in the next. Perhaps Wharton and Stillé were puzzled by the drawing of the subject included alongside Neill’s article.
Following Neill’s description, the subject’s picture revealed an athletic male physique: broad shoulders, narrow hips, and muscular limbs. She had breasts and a smooth face, and the genitals looked more male than female, as Neill originally suggested. A second drawing depicted a closer view of the penis/clitoris with a vaginal opening underneath. Perhaps Dr. Neill was right to conclude that the person was “certainly entitled to the term hermaphrodite.” The visual portrayal of the subject is as confusing as the genitals; the coroner had said that the subject died of drunkenness and exposure and lived “among the degraded blacks in the lower portion of the city.” The figure here looks more like a Greek god/goddess than someone devastated by alcohol and poverty. Furthermore, as the subject arrived at the university already dead, the image of her posing elegantly, standing against a table, adds to the general uncertainty of the case.
Wharton and Stillé recognized that the definition of hermaphroditism was shifting, though their language betrays a continued commitment to the monster motif. “Hermaphroditism” was no longer used only to describe the “perfect” union of male and female organs in one individual, which, along with self-impregnation, seemed impossible. By the mid-nineteenth century, the term was coming to be used more broadly without the qualifying “perfect” to describe, as they put it, “all those cases in which doubts exist concerning the real sex, in consequence of some aberration from the normal type of the genital organs.” This development, in turn, reflects the growing acknowledgement within the medical community that it was often difficult to determine a person’s sex, particularly at a young age or even, as in Neill’s case above, after death. “We can only hope to approximate to the truth,” noted Wharton and Stillé, “by observing whether there is not some regularity in the freaks of nature, and thus discover, if possible, some uniform correspondence between the visible deviations and those which are hidden from our view.” Urging restraint, Wharton and Stillé cautioned against a hasty pronunciation of a person’s “true” sex, a prudence that went largely unheeded in the twentieth century.
Hermaphrodites and Homosexuals
Those authorities who believed in the impossibility of hermaphrodites did not deny that sometimes people were born with a mixture of male and female organs. Rather, they held that, despite such bodily conformations, each person had a true sex to which he or she belonged. Their denial of hermaphrodites, then, meant simply that doctors would have to look harder to determine each patient’s core identity. If hermaphrodites were, at best, exceedingly rare, then ambiguously sexed patients were simply men or women who just needed to learn their true sex. Of course, this knowledge could lead to trouble. Suppose, for example, patient X was living as male in sexual intimacy with a woman. If a doctor decided patient X was really not a man at all, but rather a woman, then X’s relationship was homosexual. Hermaphroditism thus had the potential of fostering homosexuality and, by association with this prohibited “vice,” with perversity and immorality, as the epigraph suggests.
In the late nineteenth century, doctors began to sort the differences between alleged hermaphrodites and homosexuals. To modern readers, the distinctions seem obvious: hermaphroditism concerned physical anomalies. Homosexuality has nothing to do with the shape of one’s genitals; it concerns sexual orientation. People born with ambiguous genitalia may or may not experience same-sex desire, just as people born with unequivocal genitalia may or may not. Though some scientists today search for genetic or hormonal clues to homosexuality’s origin, thus connecting propensity to biology, the predominant view is that same-sex desire is not dependent on manifest physical traits. That is, even scientists investigating biological causes do not typically study genital anatomy.
In the late nineteenth and early twentieth century, some doctors drew a distinction similar to the one commonly used today: hermaphrodites necessarily had unusual genital anatomies; homosexuals did not. The divergence, however, was not clear-cut. Doctors often equated hermaphrodites and homosexuals. For example, if hermaphrodites’ genitals were ambiguous, thus masking their “true” sex, then might their sexual intercourse constitute homosexuality? And similarly, since homosexuals preferred intimacy with members of their same sex, then might they suffer from a “mental” or “psychical” hermaphroditism, a deformity centered in the brain, which is also an organ? Though possessed of “normal” genitalia, such deviants (as they were then called) might nonetheless be pushed by their hermaphroditic mental organ to feel and act transgressively. Some adherents to this opinion wanted to amend negative views about same-sex desire by proving it was congenital—just as many today assert that sexual proclivity is biological, innate, and immutable rather than “a choice” and hence immoral. But far more physicians viewed homosexuality with disgust and had no such agenda; for them homosexuality was a freely chosen and vile outrage. In the process, then, of conflating the categories, hermaphroditism became further entangled with negative associations of homosexual degeneracy. Whereas in earlier years it was connected with monstrosity and duplicity, in the late nineteenth and early twentieth centuries, hermaphroditism became virtually synonymous with immorality and perversion.
Both these tendencies—to equate hermaphroditism with monstrosity or with social and sexual deviancy—reflected the persistent power of Western society’s binary conception of sexuality. And many of the questions that had animated the medical and legal literature in the eighteenth and early nineteenth centuries thus continued to hold sway into the modern era: Could one legitimately remain outside this inflexible bifurcation? If not, and one had to be designated female or male, how would that choice be decided? Would doctors choose for their patients? How would doctors deal with patients whom they believed were living as the wrong gender? Would they persuade patients to switch genders in midlife? Would they urge surgery to make their patients’ bodies fit more neatly into one or the other category? And how would people whose genitals were under scrutiny respond? Would they listen to their doctors? Or would they ignore their advice and continue living their lives as they chose? What would be the criteria for choosing a gender? Would doctors and patients make their decisions based on secondary sex characteristics, on gender performance? How important would sexual desire come to be in the assessment?
In 1897 Dr. William Lee Howard published an article called “Psychical Hermaphroditism” in which he separated inversion from consideration of unusual genitalia but nonetheless applied the term “hermaphroditism” to what he saw as “perversion.” According to Howard, the genitals of the “pervert” are typically “normal in appearance and function.” Inversion, then, was purely a psychological condition and not something structural at all. Like hermaphroditism, though, inversion was congenital, rather than acquired. Howard quoted one of his patients, a thirty-year-old man, who said he loved men just as other men loved women. The patient explained, “I can define my disposition no better than to say that I seem to be a female in a perfectly formed male body, for, so far as I know, I am a well-formed man, capable of performing all of man’s functions sexually. Yet as far back as I can remember, surely as young as nine years, I seemed to have the strongest possible desire to be a girl, and used to wonder if by some peculiar magic I might not be transformed. I played with dolls; girls were my companions; their tastes were my tastes; flowers and millinery interested me and do now.” Thus a new twist on hermaphroditism emerged, an inversion that involved the mind rather than strictly the body.
By the end of the nineteenth century, “psychosexual,” “mental,” or “psychical” hermaphroditism were all terms doctors used to describe patients who admitted to same-sex desire or cross-gender identification. People with normal genitalia who confessed to an “inverted” gender identity, like Dr. Howard’s patient above, were termed “hermaphrodites” as were people with ambiguous genitalia, whatever their sexual inclinations. Hermaphroditism became a term that could be used to describe either a physical condition (with or without homosexuality) or a psychological one involving same-sex desire.
In the medical discussion of hermaphroditism, we can see how, rather than merely describing atypical conformation, doctors created the notion of the freakish or perverse hermaphrodite. The hermaphrodite could be treated and normalized through surgical procedures, which would culminate not only in satisfactory genitalia, but in the performance of the suitable social role in marriage. Surgeries typically offered to women included opening of vaginal occlusion, testicular removal, and clitoral excision. Surgeries for men with hypospadias included straightening the penis and extending the urethra through the penis. All of these operations made the patients “fitter” for heterosexual penetration, and the doctors wrote their case studies with intercourse and marriage as the primary indicator of a successful outcome.
In the early twentieth century, it was still all but impossible for a person to be labeled a true hermaphrodite, and doctors continued to search for clues as to a person’s true sex. Many of the themes surrounding hermaphrodites endured from the colonial period, including the tendency to simply deny hermaphroditism. The motifs of monstrosity, mistaken sex, deliberate deceit or fraud, and the potential for celibacy or non-heterosexual intimacy continued to capture doctors’ imaginations and arouse their anxiety. But other notions, such as blaming mothers’ harmful thoughts or questioning whether or not those born with unusual anatomies had souls, gradually receded. As in earlier periods, a commitment to heterosexual marriage reinforced binary notions of human sex. Doctors believed that surgery was warranted in many of these cases, not necessarily for the health, comfort, or pleasure of the patient, but to preclude the undesirable potential for homosexual sex. According to some physicians, even life-long celibacy, via castration, was preferable to homosexuality. Into the twentieth century, doctors’ primary motivation was not to enable the patient to have the partner s/he wanted but was rather to affirm normative conceptions of marriage and sex.
Further Reading:
For a historical interpretation of intersex that focuses on England and France, see Alice Domurat Dreger, Hermaphrodites and the Medical Invention of Sex (Cambridge, Mass., 1998). If you’re interested in the nineteenth century in particular, see Christina Matta, “Ambiguous Bodies and Deviant Sexualities: Hermaphrodites, Homosexuality, and Surgery in the United States, 1850-1904,” Perspectives in Biology and Medicine 48:1 (2005): 74-83. For a broader chronological perspective, see my “Impossible Hermaphrodites: Intersex in America, 1620-1960,” Journal of American History 92:2 (2005): 411-441. For a contemporary examination of the medical, political, and gendered issues regarding intersex, see Suzanne Kessler, Lessons from the Intersexed (New Brunswick, N.J., 1998). For a personal account that highlights the shame and secrecy that attends medical interference, see Cheryl Chase, “Hermaphrodites with Attitude: Mapping the Emergence of Intersex Political Activism,” GLQ 4:2 (1998): 189-211.
Regarding surgical solutions to genital anomalies, “correction” may have been the goal, but as many intersex people have noted, surgery sometimes brought more harm than good, including further operations to eliminate scar tissue and procedures that necessarily resulted in the loss of sexual sensation. Today, intersex activist groups such as ISNA (Intersex Society of North America) advocate delaying surgery until a patient is old enough to make these irrevocable decisions for himself or herself. See Howard Devore, “Growing up in the Surgical Maelstrom,” and Sven Nicholson, “Take Charge! A Guide to Home Catheterization,” both in Alice Domurat Dreger, ed., Intersex in the Age of Ethics (Hagerstown, Md., 1999): 78-81, 201-08.
This article originally appeared in issue 8.2 (July, 2008).
Elizabeth Reis is completing a book titled Bodies in Doubt: An American History of Intersex, to be published by Johns Hopkins University Press. She is an associate professor of women’s and gender studies and history at the University of Oregon.